This post was originally published on this site
Being out of work isn’t bad just for your finances: It’s bad for your health. Losing a job can cause depression, anxiety and other mental-health problems. Research also consistently shows that job loss and unemployment—even just for a few months—are associated with poorer physical health as well, including increased risks for cardiovascular disease, hospitalization and death. These risks can endure for years or even decades after a person returns to work.
As researchers who study the health effects of job loss and unemployment, we see many reasons to worry that the next wave of health problems linked to COVID-19 will not come directly from the virus itself, or the strain it places on health systems, but from its effect on the labor market.
During the first six months of the COVID-19 pandemic, 25% of U.S. adults said they or someone in their household lost their job because of the pandemic. Among those who said they lost a job, half reported they were still unemployed six months later. Racial and ethnic minorities have been hit hardest by pandemic-driven job losses and deaths. These communities already face longstanding structural inequities in living and working conditions that affect their job prospects and may shape their financial recovery.
The health impacts of job loss
It’s not hard to see why losing a job, followed by a period of unemployment, can be bad for a person’s health. The initial months following a job loss can reduce social support by straining people’s finances and psychological well-being and limiting their social interactions. People who lose their health insurance along with their job may not seek medical attention when illness arises. The stresses caused by losing a job can also lead people to increase the use of alcohol or drugs, eat poorly, exercise less or develop bad sleep patterns.
These risks persist even if someone receives unemployment benefits or gets another job relatively quickly. Some research shows a few months of unemployment may be associated with worse long-term health and well-being. One study found that in the year after the participants lost their jobs, death rates among them were as much as two times higher regardless of whether and when they got a new one, and remained 10%-15% higher than expected for the next 20 years. If this rate of increased risk continued indefinitely, the authors noted, losing a job at age 40 could reduce life expectancy by 1-1 ½ years.
Other research has associated job loss with a higher risk of conditions including hypertension and arthritis, and a twofold higher risk of heart attack and stroke. And that’s not because people in poor health are more likely to lose their jobs. Our 2007 analysis showed that even after removing the influence of baseline health and social background, people who lost their jobs were still more likely to report poor health.
Why pandemic-driven job loss may be the next health crisis
While some of the data on which we base our concern come from other economic recessions and downturns, such as the Great Recession from 2007 to 2009, we expect that there could be even worse outcomes in the wake of COVID-19. The peak unemployment rate during the Great Recession was 10%, while the peak unemployment rate in 2020 was almost 15%. Economic recovery is more precarious when pandemic restrictions are still in place, and some business operations have changed permanently, making it harder for some laid-off workers to regain their old jobs.
Moreover, many of those who became seriously ill with COVID-19 are experiencing slow recoveries. They may not be able to work at their earlier capacities for some time. Other adults may need to take on new caregiver responsibilities because kin have remained ill, or died and left behind others who need care.
Already, preliminary analyses are emerging about the potential health effects of COVID-related unemployment, particularly among vulnerable populations. In a recent New Zealand study, the researchers estimate that pandemic-related job loss could cause a 1% rise in overall cardiovascular disease rates for each additional 1% increase in unemployment. Among the nation’s more vulnerable Indigenous Māori population, however, the disease rate rose to 4% for each 1% increase in unemployment. The authors’ model also suggests that the health effects of pandemic unemployment will persist over the next two decades.
This suggests the need for more robust support for people who are out of work, including continued health insurance coverage, to help buffer the economic toll of job loss and thereby mitigate some of its health consequences. The U.S. has some threads of a social safety net, such as up to 26 weeks of unemployment benefits in most states, and Congress created extra pandemic help when it passed the CARES Act in 2020. But these weren’t enough to prevent a huge increase in food insecurity and use of food pantries last year.
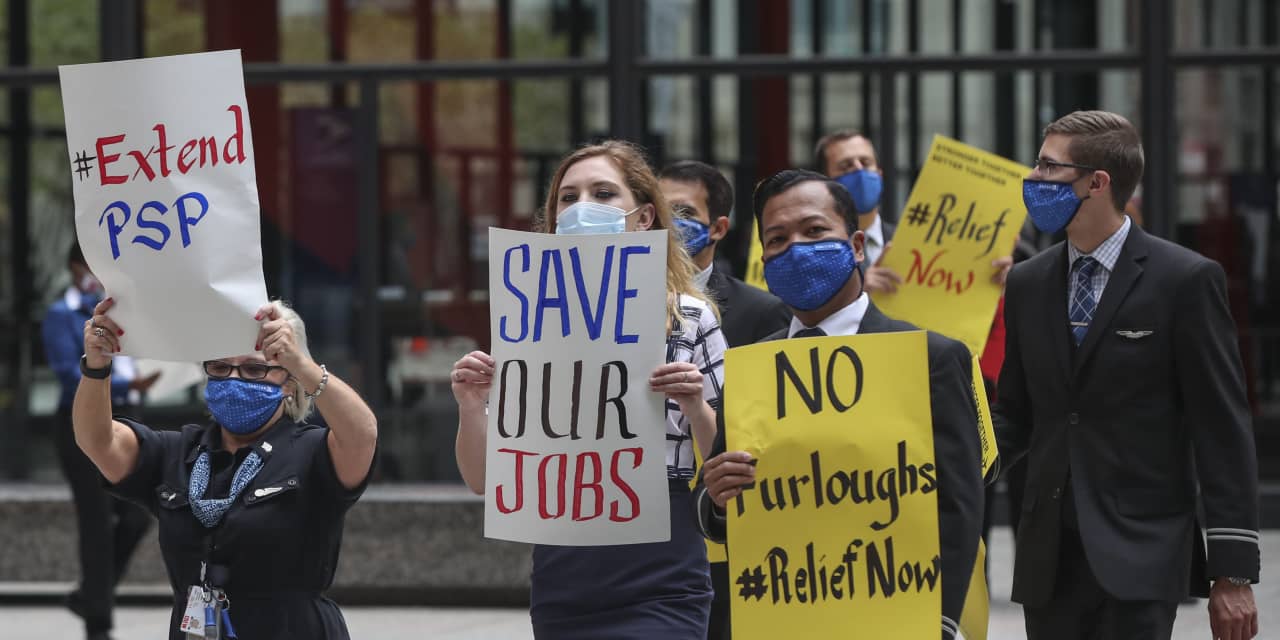
Given the potentially long-term negative effects of job loss on health, one way to protect workers may be helping companies to not lay them off. Policy makers should continue to direct resources toward employers that keep businesses going and workers employed. If layoffs are inevitable, then create incentives to rehire laid-off workers as soon as possible. In California, for instance, Gov. Gavin Newsom signed a bill in April requiring companies in hard-hit industries such as hotel and event management to rehire workers who were laid off during the pandemic when jobs become available.
To address all the health consequences of the pandemic, we believe one must think broadly about interventions and policies. We must recognize the wide scope of job losses across households and industries, not just in workplaces making media headlines, and the unequal burden felt by workers already disadvantaged before COVID-19. The real solution lies in not just getting back to work, but getting Americans into secure jobs that pay a living wage and allow economic recovery alongside the healing of people and health care systems.
Jennie E. Brand is professor of sociology and statistics at the University of California, Los Angeles. Sarah A. Burgard is professor of sociology a the University of Michigan.
This article was produced in collaboration with Knowable Magazine, a digital publication covering science and its emerging frontiers. It was originally published by The Conversation. — Why widespread health woes could follow from pandemic-driven job losses.
More from MarketWatch:
Ending enhanced unemployment benefits alone won’t get people back to work, SF Fed research suggests
Anne Case and Angus Deaton: Deaths of despair will surge again once COVID-19 recedes

