This post was originally published on this site
Private equity firms and real estate investment trusts involved in the long-term care industry are coming under new scrutiny from federal regulators.
The U.S. Department of Health and Human Services on Monday announced a proposed rule requiring nursing homes to disclose new ownership and management details, including ties with any private-equity firms or REITs and the names of individuals or entities providing administrative or clinical consulting services to the facilities.
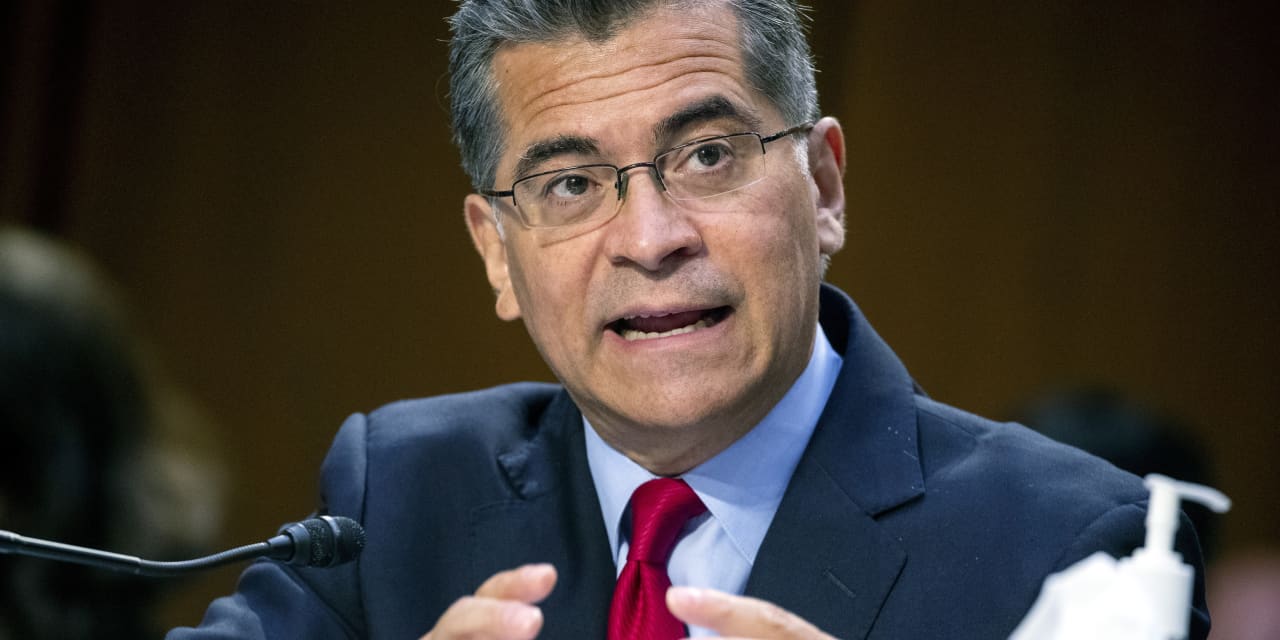
“We’re pursuing every avenue we can to shine a light on this industry,” Health and Human Services Secretary Xavier Becerra said on a call with reporters Monday.
The move comes after the pandemic exposed serious gaps in the care provided at the nation’s roughly 15,000 nursing homes as well as spotty oversight of facility owners and operators, who are often entwined in complex ownership structures that are not fully reflected in data collected by regulators.
“For too long, one of the barriers to accountability has been a lack of transparency around who owns and operates nursing homes,” Bharat Ramamurti, deputy director of the White House National Economic Council, said on the call Monday. If finalized, the new rule will help change that, he said. The new ownership and management data collected will also be publicly reported, helping families make more informed choices, he said.
A string of academic studies in recent years have found links between private equity ownership and poor outcomes for residents, including higher rates of preventable hospitalization and death. Researchers haven’t looked as closely at how care may be impacted by healthcare REITs, which in some cases buy nursing home real estate and lease it back to the facility, because they’re widely seen only as landlords.
But a study published last month in Health Affairs found evidence that some REIT-owned nursing homes replaced more expensive, skilled registered nurse staffing with cheaper, less-skilled staff. Academic researchers have also raised concerns about nursing homes buying management, therapy or other services or paying rent to related parties, saying this allows ownership groups to hide profits extracted from the facilities.
Rule would implement a provision of the Affordable Care Act
The new HHS rule proposal would implement a section of the Affordable Care Act, which was signed into law about 13 years ago. Throughout the pandemic, long-term care experts have urged the Centers for Medicare and Medicaid Services, the federal agency that oversees nursing homes, to ensure the law is enforced, including requiring full ownership details.
Federal officials on Monday underscored the importance of clear ownership disclosure as nursing homes change hands more frequently. The number of ownership changes has generally trended upward since 2016, and nursing homes with lower quality ratings are sold more often than those with higher ratings, according to an HHS report.
“What’s absolutely true is that we see more risk, that we see more harm when nursing homes change ownership,” Jon Blum, CMS principal deputy administrator and chief operating officer, said on the call Monday. “They can change owners to companies that don’t have experience, that don’t have really the knowledge, the staff” to ensure high-quality care, he said.
The rule proposal is part of a broader Biden administration nursing-home reform agenda, announced early last year, which also aims to achieve better funding for health and safety inspections and a minimum staffing requirement, among other measures. Nursing-home industry trade group American Health Care Association/National Center for Assisted Living has said a minimum staffing mandate “would impose arbitrary staffing ratios that would be impossible for providers to meet considering the current labor shortage and lack of government funding.”
But data collected under the new proposed rule could help inform the regulatory response to such industry resistance to reform, CMS’s Blum said on the call Monday. “As we think about policies going forward to fulfill the President’s commitment, we will now have better information to understand or even to refute arguments that the nursing home industry can’t afford these changes,” Blum said.

