This post was originally published on this site
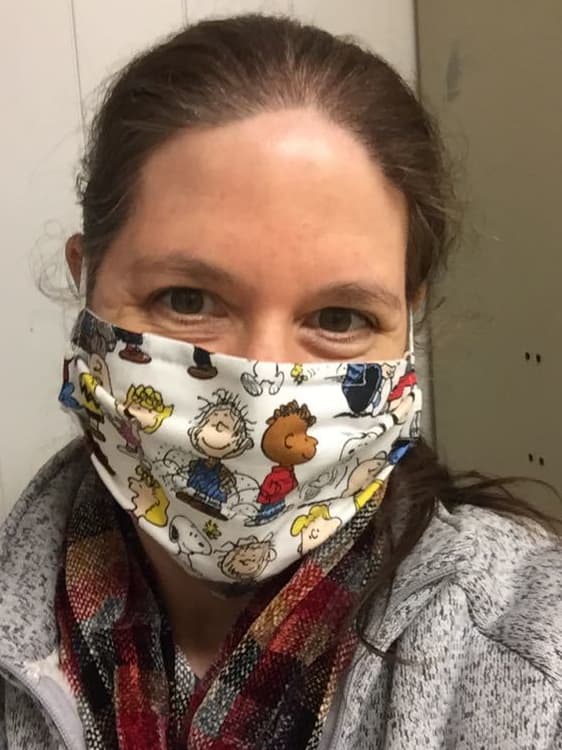
Heather-Elizabeth Brown, a corporate trainer and volunteer police chaplain who lives outside of Detroit, Mich., never expected to be drafting her will at 35.
But there she was in a hospital room last April, writing on a napkin: Her prized book collection should go to her best friend Niqui. Her makeup and hair supplies should go to her best friend Golda. Any liquid assets not kept or sold should be divided among her seven living godchildren. Although it wasn’t a legal will, she signed the napkin as a testament to her personal wishes, and tucked it into the top of her boot.
Brown, who had been hospitalized with COVID-19, would soon be placed in a medically induced coma and put on a ventilator for 31 days. In total, she would spend nearly 120 days in the hospital. The ordeal would leave her with ongoing physical, emotional and psychological challenges, plus tens of thousands of dollars in medical debt.
“
Long haulers, as they’re often called, have symptoms that range in severity and can include neurological damage, fatigue, headaches, shortness of breath and joint pain.
”
Brown, now 36, is part of a still little-understood cohort of people who survived COVID-19 but continue to deal with a range of health problems — and accompanying financial concerns — months later.
Long haulers, as they’re often called, have symptoms that range in severity and can include neurological damage, fatigue, headaches, shortness of breath and joint pain. A recent JAMA Network Open research letter found that about 30% of COVID-19 survivors followed for up to nine months reported “persistent symptoms”; an earlier U.K. study estimated “Long Covid” patients make up about 10% of people who have tested positive for the coronavirus.
The National Institutes of Health announced an initiative in February to study causes, prevention and treatment for “Long Covid,” which does not yet have a formal name in the U.S.
As they enter year two of the pandemic uncertain about a path to recovery, many long haulers are also reevaluating their household finances, family planning, retirement prospects and life goals — and redefining their priorities going forward.
“Everything I’ve reassessed because of COVID — because of how close I came to death, and because of how much has changed in [my] life on the other side as a long hauler,” Brown told MarketWatch. “I look at everything with a different lens now.”
‘Everything now is about coverage’
Nearly a year after Brown was hospitalized, she works from home and still deals with fatigue, diminished breathing capacity, “brain fog,” chronic pain and mobility issues. Life is much slower now; her actions more measured and planned to accommodate a reduced energy level. “Before, I was always on the go — always moving, always someplace, always doing something, always helping or volunteering,” she said. “Now I don’t have that ability to do that.”
Brown says her near-death experience led her to value her bonds with family and close friends even more (she feared a FaceTime
AAPL,
call with her family before going on the ventilator could be her last), and reassess her relationships with some other people.
Brown, who is currently single, also has concerns about how her long-hauler condition squares with her now-intensified desire to have children — including the prospect of dating during a pandemic with health challenges, the physical aspects of carrying a child, and the financial aspects of starting a family. “There are a lot of things that we don’t know when it comes to [Long] Covid and having a child,” she said.
Despite “phenomenal” health insurance that has covered a lot of her care, Brown now has five-figure medical debt that continues to grow due to visits to specialists. “The cost is astronomical — astronomical — for recovery,” she said. “And I don’t have a plan for how to pay this back.” For now, she said, she’s focusing on her recovery and taking the financial piece step by step.
The experience has impacted her finances in at least one positive way: a newfound drive to plan for all eventualities. Brown went back through all of her insurance plans to make sure she selected “the highest level on everything,” or the most comprehensive coverage possible. It’s impossible to control everything, she acknowledged — but “what you can try to control, you should.”
“I look at everything as an opportunity to plan for the future,” she said. “Everything now is about coverage.”
After her relatively mild case of the coronavirus, Robin Lagua says her body is ‘not the same as before.’
Courtesy of Robin Lagua
‘I’m just living for now’
The pandemic has been “very, very stressful for the grocery business,” says Robin Lagua of Edgewood, Wash., who has worked as a grocery-store cashier for 14 years. While Lagua, 52, has been vigilant about masking up, she and her 22-year-old son, who works as a produce clerk in the same store, both tested positive for the virus in late July. (She believes they caught it from a visitor to their home.)
After her relatively mild case of the coronavirus, Lagua says her body is “not the same as before.” Last fall, she developed a laryngospasm that produced coughing fits (which have lessened over time) and leg pain. In January, she developed a sensation that left her tongue feeling burnt. She sometimes gets easily winded, finds herself “really exhausted” some days, and is now more prone to body aches. “It just seems like I keep getting one thing after another,” she said.
Lagua, a mother of three who lost her husband to liver cancer 12 years ago, largely supports herself and her son, who makes minimum wage. After her husband’s death, she lost her house and claimed bankruptcy. Lagua lives frugally and drives an old car; she moves every few years when she can’t afford rent hikes. “It’s OK, but I struggle,” she said. She has no retirement savings.
But living as a widow in “survivor mode” for the past decade-plus made Lagua more resilient, she said, steeling her for COVID-19 and her subsequent long-hauler status. And despite her financial strain, Lagua said she was more concerned with the health repercussions of the coronavirus.
“It made me realize I have to enjoy whatever time I have with my son,” she said. “The main thing is just your emotional and physical being — because if you don’t have that, no money in the world is going to make you feel better.”
After losing her husband and living with Long Covid, “I’m just living for now,” Lagua added. “Or ‘one day at a time,’ as my late husband would say.”

Lynus Parker, a hiking, biking, fishing, yoga and golf enthusiast, is living in what he calls ‘a new normal.’
Courtesy of Lynus Parker
‘You can’t live your life post-COVID looking over your shoulder’
Lynus Parker of Novi, Mich., will always remember the moment last April when a doctor said intubation was his best chance for survival against the coronavirus. “I was like, ‘What? Survival!’ … I’m the healthiest guy I know,” Parker, a hiking, biking, fishing, yoga and golf enthusiast in his 50s, told MarketWatch. “I just prayed and called my wife and daughter and went under.”
Parker, who was told it would only be three to four days, spent 32 days on a ventilator in and out of a coma; he woke up to find that doctors had performed a tracheostomy to help him breathe. He spent a month and a half transitioning to unassisted breathing and another two weeks in rehabilitation. (Parker later chronicled his journey in greater detail in a video diary.) By the time he returned home in July, he had lost about 55 pounds.
The whole experience left him with post-traumatic stress disorder, he said. He created a Facebook
FB,
support group for long haulers last fall “to try to shine some light on this dark situation”; it now counts more than 700 members.
Today, he has damaged lungs, a paralyzed vocal cord, paralysis of the right side of his diaphragm, and sleep apnea from the diaphragm issue, which has caused headaches. But Parker, a global account executive for a software company, has resumed full-time remote work. “I’m overcoming. I’m working. I’m just dealing with it,” he said. “I’m really fortunate that I did maintain my role and they believed in me … otherwise, this would be a completely different type of discussion.”
Parker says it’s critical that the vast array of symptoms associated with long haulers be documented and categorized, so they can be taken into account for treatment and insurance purposes. He worries about the potential for hiring discrimination against COVID-19 survivors. Meanwhile, Parker and his wife, who was laid off last April due to the pandemic and has been advocating for him throughout his recovery, have had to reprioritize their spending as medical bills continue to roll in.
“It’s not that there weren’t [financial constraints] before, but the money we were saving was going toward retirement — and now I don’t have that same liberty of putting stuff away. That means I have to work longer,” he said. “So it’s interrupted my schedule and savings plan to account for some of that.”
The experience, Parker said, taught him what’s most important: his family and his health. He’s living in what he calls “a new normal.” “You can’t live your life post-COVID looking over your shoulder at what you used to have,” he said. “You can only move forward if you’re looking forward.”

Words that Emily Haozous uses to describe life as a long hauler include ‘stagnant,’ ‘pretty limited’ and ‘on hold.’
Courtesy of Emily Haozous
‘I wake up and I feel the same’
Emily Haozous, a nurse researcher and enrolled member of the Chiricahua Fort Sill Apache tribe who lives in Santa Fe, N.M., is used to being an observer, helper and information source. Her research has lately centered on Native Americans and COVID-19, which has hospitalized and killed American Indian and Alaska Native individuals at disproportionate rates.
“Having Long Covid has put me behind a computer instead of on the front line, which is where I would like to be — volunteering, helping out wherever I’m needed,” Haozous, 47, told MarketWatch. “So I feel totally detached from everyone. Just watching and documenting. It’s truly awful.”
Haozous and her family contracted COVID-19 last March during a spring-break trip to New York City. She says she went “up and down” for weeks with cough, shortness of breath, low-grade fever, chills, aches and fatigue. “In June or July, I started to think, ‘This isn’t just COVID — this is a really bad joke,’” she said. “Every time I felt better, I’d be like, ‘Oh, it’s gone.’ I would go for a walk or try to exercise, and it would put me right back on the couch.”
Words Haozous uses to describe life as a long hauler include “stagnant,” “pretty limited” and “on hold.” She recently woke up and told her husband, “Happy Groundhog Day.” “Before, if I was sick, I would wake up and do this body check and say, ‘Oh, I feel better today,’” she said. “But now I wake up and I feel the same. I feel just as awful as the day before. And I’m not getting better.”
Haozous feels grateful to have been able to continue working from home. These days, she deals with fatigue and brain fog, along with regular cold symptoms like sore throat, low-grade headache and a run-down, stuffy feeling. She spends weekends recuperating so she can make it through the work week, and worries about getting sicker or experiencing chronic repercussions from COVID-19.
“I’m just trying to work and keep doing as many hours as I can now, just in case. And I’m not making any big purchases, or making any plans to move or anything,” Haozous said. The amount of money it will eventually cost to send her two teen sons to college is “horrifying,” she added, “and this is not the time for me to be sick and not be able to work extra hours to save up as much as possible.”
She has not, however, gone out of her way to seek treatment for her ongoing symptoms. Haozous recalls attending a conference session on long haulers, where she learned many of them had no “measurable clinical indicators.” After that, she said, she decided she didn’t want to undergo expensive and time-consuming scans and tests only to undermine her own credibility in the eyes of the healthcare system.
“I really hope that we can get attention to this problem, and I really hope that it happens soon,” she said.
‘My world was turned upside down’
Nicole, a 34-year-old in the Washington, D.C. area who asked to be identified only by her middle name to avoid potential repercussions from her employer, married her husband the fall before the pandemic hit. But the trials of 2020 meant they would burn through their honeymoon fund to pay bills, and put their plans for having kids on hold.
“We went from this really high point in our lives with really our whole future ahead of us,” she said, “into this hellfire of a year.”
Nicole tested positive for the virus in September; she endured a relatively mild case, though the symptoms “were no cake walk.” But toward the end of her illness, she began experiencing excruciating migraines that put her out of commission for a day or two. Extreme fatigue and brain fog also set in. “As a healthy 34-year-old woman, it was like my world was turned upside down,” said Nicole, who was previously a “highly active” barre instructor.
Nicole was unable to work from mid-September through late January, and while she was able to take some time off through her employer, she was denied short-term disability benefits because Long Covid wasn’t recognized as a disability. Losing about two months’ worth of wages meant monetary wedding gifts, savings and their honeymoon fund went toward bills and mortgage payments.
“I feel so thankful that we did have that, because I know so many others are in much worse circumstances,” she said. Still, financial uncertainty bred depression and anxiety, she added.
Nicole, who has paid nearly $5,000 out of pocket for various tests, visits, medications and supplements, still has about $2,000 in medical debt. She and her husband have delayed planning for their first child, opting to wait until her health improves, their finances stabilize, and they have an opportunity to travel before growing their family.
The migraines seem to be coming less frequently of late. Nicole often has trouble falling or staying asleep. She’s participating in a COVID-19 recovery program that offers long haulers services from a range of specialists; while many of her tests have come back “normal,” neuropsychological tests have shown cognitive impairments with her memory. “They were explaining to me that registering and uncoding things has become really difficult for me,” she said. “New information hasn’t been sticking.”
Nicole said her mind goes to dark places sometimes. But she feels hopeful when she sees members of her long-hauler Facebook support group “graduate” and leave the group because their condition has improved.
“Some people are getting better,” she said. “Those are the things that I try to cling on to.”

